Good assessment skill is paramount in providing quality nursing care. There is the reason why Assessment is the first step in the nursing process and is incorporated in every phase. In assessment nurses can gather pertinent information from the patient's health status so as to have a good overview of the patient's condition to be able to formulate a nursing diagnosis and even help doctors to come up with their medical diagnosis- much more it help the whole health care team.
The health history focuses on the physical and functional problems of the patient and the effect of these problems on his or her life. The reason the patient is seeking health care often is related to one of the following: dyspnea (shortness of breath), pain, accumulation of mucus, wheezing, hemoptysis (blood spit up from the respiratory tract), edema of the ankles and feet, cough, and general fatigue and weakness.
In addition to identifying the chief reason why the patient is seeking health care, the nurse tries to determine when the health problem or symptom started, how long it lasted, if it was relieved at any time, and how relief was obtained. The nurse collects information about precipitating factors, duration, severity, and associated
factors or symptoms and also assesses for risk factors and genetic factors that may contribute to the patient’s lung condition.
The nurse assesses the impact of signs and symptoms on the patient’s ability to perform activities of daily living and to participate in usual work and family activities. In addition, psychosocial factors that may affect the patient are explored. These factors include anxiety, role changes, family relationships, financial problems, employment status, and the strategies the patient uses to cope with them.
Many respiratory diseases are chronic and progressively debilitating. Therefore, ongoing assessment of the patient’s physical abilities, psychosocial supports, and quality of life is needed to plan appropriate interventions. It is important for the patient with a respiratory disorder to understand the condition and to be
familiar with necessary self-care interventions. The nurse evaluates these factors over time and provides education as needed.
Signs and Symptoms
The major signs and symptoms of respiratory disease are dyspnea, cough, sputum production, chest pain, wheezing, clubbing of the fingers, hemoptysis, and cyanosis. These clinical manifestations are related to the duration and severity of the disease.
DYSPNEA
Dyspnea (difficult or labored breathing, shortness of breath) is a symptom common to many pulmonary and cardiac disorders, particularly when there is decreased lung compliance or increased airway resistance. The right ventricle of the heart will be affected ultimately by lung disease because it must pump blood through
the lungs against greater resistance. It may also be associated with neurologic or neuromuscular disorders such as myasthenia gravis, Guillain-Barré syndrome, or muscular dystrophy.
Clinical Significance. In general, acute diseases of the lungs produce a more severe grade of dyspnea than do chronic diseases. Sudden dyspnea in a healthy person may indicate pneumothorax (air in the pleural cavity), acute respiratory obstruction, or ARDS. In immobilized patients, sudden dyspnea may denote pulmonary embolism. Orthopnea (inability to breathe easily except in an upright position) may be found in patients with heart disease and occasionally in patients with chronic obstructive pulmonary disease (COPD); dyspnea with an expiratory wheeze occurs with COPD. Noisy breathing may result from a narrowing of the airway or localized obstruction of a major bronchus by a tumor or foreign body. The presence of both inspiratory and expiratory wheezing usually signifies asthma if the patient does not have heart failure.
The circumstance that produces the dyspnea must be determined. Therefore, it is important to ask the patient the following questions:
• How much exertion triggers shortness of breath?
• Is there an associated cough?
• Is dyspnea related to other symptoms?
• Was the onset of shortness of breath sudden or gradual?
• At what time of day or night does the dyspnea occur?
• Is the shortness of breath worse when the patient is flat in bed?
• Does the shortness of breath occur at rest? With exercise? Running? Climbing stairs?
• Is the shortness of breath worse while walking? If so, when walking how far? How fast?
Relief Measures. The management of dyspnea is aimed at identifying and correcting its cause. Relief of the symptom sometimes is achieved by placing the patient at rest with the head elevated (high Fowler’s position) and, in severe cases, by administering oxygen.
COUGH
Cough results from irritation of the mucous membranes anywhere in the respiratory tract. The stimulus producing a cough may arise from an infectious process or from an airborne irritant, such as smoke, smog, dust, or a gas. The cough is the patient’s chief protection against the accumulation of secretions in the bronchi and bronchioles.
Clinical Significance. Cough may indicate serious pulmonary disease. The nurse needs to evaluate the character of the cough is it dry, hacking, brassy, wheezing, loose, or severe? A dry, irritative cough is characteristic of an upper respiratory tract infection of viral origin or may be a side effect of angiotensin-converting enzyme (ACE) inhibitor therapy. Laryngotracheitis causes an irritative, high-pitched cough. Tracheal lesions produce a brassy cough. A severe or changing cough may indicate bronchogenic carcinoma. Pleuritic chest pain accompanying coughing may indicate pleural or chest wall (musculoskeletal) involvement
The time of coughing is also noted. Coughing at night may herald the onset of left-sided heart failure or bronchial asthma. A cough in the morning with sputum production may indicate bronchitis. A cough that worsens when the patient is supine suggests postnasal drip (sinusitis). Coughing after food intake may
indicate aspiration of material into the tracheobronchial tree. A cough of recent onset is usually from an acute infection.
SPUTUM PRODUCTION
A patient who coughs long enough almost invariably produces sputum. Violent coughing causes bronchial spasm, obstruction, and further irritation of the bronchi and may result in syncope (fainting). A severe, repeated, or uncontrolled cough that is nonproductive is exhausting and potentially harmful. Sputum production is the reaction of the lungs to any constantly recurring irritant. It also may be associated with a nasal discharge.
Clinical Significance. A profuse amount of purulent sputum (thick and yellow, green, or rust-colored) or a change in color of the sputum probably indicates a bacterial infection. Thin, mucoid sputum frequently results from viral bronchitis. A gradual increase of sputum over time may indicate the presence of chronic bronchitis or bronchiectasis. Pink-tinged mucoid sputum suggests a lung tumor. Profuse, frothy, pink material, often welling up into the throat, may indicate pulmonary edema. Foul-smelling sputum and bad breath point to the presence of a lung abscess, bronchiectasis, or an infection caused by fusospirochetal or other anaerobic organisms.
Relief Measures. If the sputum is too thick for the patient to expectorate, it is necessary to decrease its viscosity by increasing its water content through adequate hydration (drinking water) and inhalation of aerosolized solutions, which may be delivered by any type of nebulizer. Strategies to assist the patient to cough productively are discussed later in this chapter.
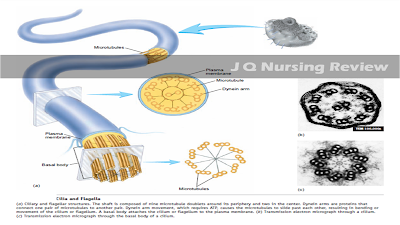
Smoking is contraindicated with excessive sputum production because it interferes with ciliary action, increases bronchial secretions, causes inflammation and hyperplasia of the mucous membranes, and reduces production of surfactant. Thus, smoking impairs bronchial drainage. When the person stops smoking,
sputum volume decreases and resistance to bronchial infections increases.
The patient’s appetite may decrease because of the odor of the sputum or the taste it leaves in the mouth. The nurse encourages adequate oral hygiene and wise selection of food, measures that will stimulate appetite. In addition, the nurse encourages the patient and family to remove sputum cups, emesis basins, and soiled
tissues before mealtime. Encouraging the patient to drink citrus juices at the beginning of the meal may increase the palatability of the rest of the meal because these juices cleanse the palate of the sputum taste.
CHEST PAIN
Chest pain or discomfort may be associated with pulmonary or cardiac disease. Chest pain associated with pulmonary conditions may be sharp, stabbing, and intermittent, or it may be dull, aching, and persistent. The pain usually is felt on the side where the pathologic process is located, but it may be referred elsewhere—for example, to the neck, back, or abdomen.
Clinical Significance. Chest pain may occur with pneumonia, pulmonary embolism with lung infarction, and pleurisy. It also may be a late symptom of bronchogenic carcinoma. In carcinoma the pain may be dull and persistent because the cancer has invaded the chest wall, mediastinum, or spine.
Lung disease does not always produce thoracic pain because the lungs and the visceral pleura lack sensory nerves and are insensitive to pain stimuli. However, the parietal pleura has a rich supply of sensory nerves that are stimulated by inflammation and stretching of the membrane. Pleuritic pain from irritation of the parietal pleura is sharp and seems to “catch” on inspiration; patients often describe it as “like the stabbing of a knife.” Patients are more comfortable when they lie on the affected side as this splints the chest wall, limits expansion and contraction of the lung, and reduces the friction between the injured or diseased pleurae on that side. Pain associated with cough may be reduced manually by splinting the rib cage.
The nurse assesses the quality, intensity, and radiation of pain and identifies and explores precipitating factors, along with their relationship to the patient’s position. Also, it is important to assess the relationship of pain to the inspiratory and expiratory phases of respiration.
Relief Measures. Analgesic medications may be effective in relieving chest pain, but care must be taken not to depress the respiratory center or a productive cough, if present. Nonsteroidal anti-inflammatory drugs (NSAIDs) achieve this goal and thus are used for pleuritic pain. A regional anesthetic block may be performed to relieve extreme pain.
WHEEZING
Wheezing is often the major finding in a patient with bronchoconstriction or airway narrowing. It is heard with or without a stethoscope, depending on its location. Wheezing is a highpitched, musical sound heard mainly on expiration.
Relief Measures. Oral or inhalant bronchodilator medications reverse wheezing in most instances.
CLUBBING OF THE FINGERS
Clubbing of the fingers is a sign of lung disease found in patients with chronic hypoxic conditions, chronic lung infections, and malignancies of the lung. This finding may be manifested initially as sponginess of the nailbed and loss of the nailbed angle.
HEMOPTYSIS
Hemoptysis (expectoration of blood from the respiratory tract) is a symptom of both pulmonary and cardiac disorders. The onset of hemoptysis is usually sudden, and it may be intermittent or continuous. Signs, which vary from blood-stained sputum to a large, sudden hemorrhage, always merit investigation. The most common causes are:
• Pulmonary infection
• Carcinoma of the lung
• Abnormalities of the heart or blood vessels
• Pulmonary artery or vein abnormalities
• Pulmonary emboli and infarction
Diagnostic evaluation to determine the cause includes several studies: chest x-ray, chest angiography, and bronchoscopy. A careful history and physical examination are necessary to diagnose the underlying disease, irrespective of whether the bleeding involved a very small amount of blood in the sputum or a massive hemorrhage.
The amount of blood produced is not always proportional to the seriousness of the cause.
First, it is important to determine the source of the bleeding— the gums, nasopharynx, lungs, or stomach. The nurse may be the only witness to the episode. When documenting the bleeding episode, the nurse considers the following points:
• Bloody sputum from the nose or the nasopharynx is usually preceded by considerable sniffing, with blood possibly appearing in the nose.
• Blood from the lung is usually bright red, frothy, and mixed with sputum. Initial symptoms include a tickling sensation in the throat, a salty taste, a burning or bubbling sensation in the chest, and perhaps chest pain, in which case the patient tends to splint the bleeding side. The term “hemoptysis” is reserved for the coughing up of blood arising from a pulmonary hemorrhage. This blood has an alkaline pH (greater than 7.0).
• If the hemorrhage is in the stomach, the blood is vomited (hematemesis) rather than coughed up. Blood that has been in contact with gastric juice is sometimes so dark that it is referred to as “coffee grounds.” This blood has an acid pH (less than 7.0).
CYANOSIS
Cyanosis, a bluish coloring of the skin, is a very late indicator of hypoxia. The presence or absence of cyanosis is determined by the amount of unoxygenated hemoglobin in the blood. Cyanosis appears when there is 5 g/dL of unoxygenated hemoglobin. A patient with a hemoglobin level of 15 g/dL will not demonstrate cyanosis until 5 g/dL of that hemoglobin becomes unoxygenated, reducing the effective circulating hemoglobin to two thirds of the normal level. An anemic patient rarely manifests cyanosis, and a
polycythemic patient may appear cyanotic even if adequately oxygenated. Therefore, cyanosis is not a reliable sign of hypoxia. Assessment of cyanosis is affected by room lighting, the patient’s skin color, and the distance of the blood vessels from the surface of the skin. In the presence of a pulmonary condition, central cyanosis is assessed by observing the color of the tongue and lips. This indicates a decrease in oxygen tension in the blood. Peripheral cyanosis results from decreased blood flow to a certain area of the body, as in vasoconstriction of the nailbeds or earlobes from exposure to cold, and does not necessarily indicate a central systemic problem.